Achilles' Tendon Disorders
The Achilles tendon is a group of tough fibrous tissue that connects the calf muscles to the heel bone. It functions to lift the heel while walking or running. The two major problems associated with the Achilles tendon are:
- Achilles tendonitis: inflammation of the Achilles tendon
- Achilles tendinosis: degeneration of the Achilles tendon due to unresolved inflammation. The tendon develops minute tears or pores in the tissue, losing its unique structure.
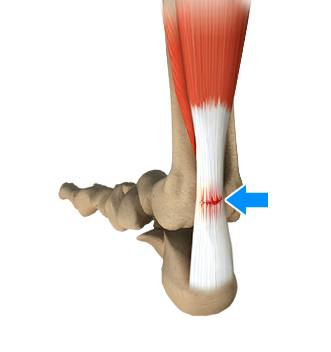
Sometimes, because of degeneration, an Achilles tendon also tears or ruptures partially or completely, causing pain or loss of movement.
What are the causes of Achilles tendon disorders?
Constant overuse or repetitive activities can cause Achilles tendon disorders. These activities exert excessive stress on the tendon and lead to micro-tears.
Participating in sports and exercises can increase your risk of developing Achilles tendon disorders. It is also commonly seen in people whose occupation puts lot of pressure on their feet and ankles. Simple movements like running, jumping, stretching and improper shoes can also result in the rupture of the tendon.
What are the associated symptoms?
Symptoms related to Achilles tendon disorders include:
- Swelling and bruising
- Mild or severe pain
- Stiffness
- Loss of strength
- Decreased movement of the ankle
- Muscle weakness or tenderness
- Difficulty in walking or standing
How are these conditions diagnosed?
Diagnosis is based on the following:
- Medical history
- Physical examination of the foot and ankle to assess movements and condition of the tendon
- Radiological investigations such as foot or ankle X-rays or MRI scans
What are the treatment options?
Treatment options depend on the duration and extent of injury to the tendon. Mild cases can be treated by the following approaches:
- Take adequate rest.
- Your doctor will prescribe medications to relieve pain and inflammation.
- Apply ice bags over a towel on the affected area for 15 to 20 minutes to reduce swelling and inflammation.
- Restrict activities that cause pain and stress for a short duration.
- Your doctor will immobilize your foot with a cast, splint, brace, walking boot or other device, to prevent movement of your leg and assist in faster healing of the tendon.
- Physical therapy modalities such as strengthening exercises, massage, ultrasound therapy, stretching and a walking rehab program are advised to improve range of motion.
- Surgery is indicated only in severe cases and depends on the age and activity level of the individual, extent of damage to the tendon, and other factors.
Strictly follow the post-treatment instructions and wear appropriate shoes for the foot type and activity as recommended by your doctor to prevent the recurrence of the condition.











